After determining benefit information during verification, staff informs the patient of their financial responsibilities. That enables the biller to collect the copay, deductible, coinsurance, or the entire sum due while the patient is at the front desk, either during check-in or medical billing cycle steps check-out. Healthray pioneers healthcare tech with innovative solutions for doctors, offering a suite of software including EMR, RIS, and HMIS. However, if the quantum isn’t zero, the charges and benefits they admit or don’t admit from the insurer should be made veritably clear.
Sommaire
Step 3: Capturing Codes

In this video, we’ll learn more about this process by breaking it down into a handful of easy-to-understand steps. Though it might ameliorate job chances, an instrument isn’t necessary to master billing, and state-by-state differences live in billing procedures. Since then, there have been at least a dozen new ICD procedure codes related to the virus and many more changes to CPT and HCPCS codes to document COVID-19 and related conditions.
The Definitive Checklist for Submitting Medical Claim Forms
The industry uses the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10) to capture diagnosis codes for billing purposes. This step will allow you to verify that you have the correct insurance information, that the patient is currently covered, and review their out-of-pocket obligations. Confirming this information will help avoid delays and billing errors later on. Once pulled, this information is translated into a claim and sent to third-party payers for reimbursement. Studies underscore the significance of unambiguous and frank communication in responding to patient inquiries, enabling prompt payments, and augmenting patient contentment in general. Well-designed patient statements facilitate an excellent patient financial experience.

Medical Claims Processing
(If the patient has secondary insurance, the biller takes the amount left over after the primary insurance returns the approved claim and sends it to the patient’s secondary insurance). Medical billing uses two sets of codes to record and classify patient/provider interactions. Called the International Classification of Diseases (ICD) codes, this set of codes corresponds to the problem or problems being evaluated or treated. The current code system is ICD-10, with an updated set of ICD-11 codes set to become the standard in 2025. Once a patient is registered, you’ll need to determine what treatments are covered by their insurance plan.
Denial management
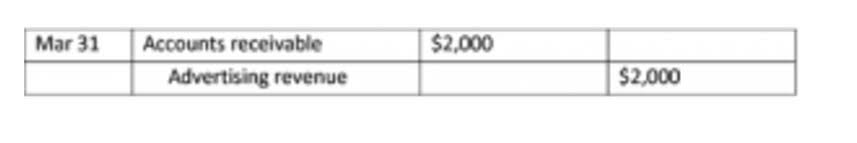
The patient will also be required to provide some sort of official identification, like a driver’s license or passport, in addition to a valid insurance card. Financial responsibility describes who https://www.bookstime.com/ owes what for a particular doctor’s visit. Once the biller has the pertinent info from the patient, that biller can then determine which services are covered under the patient’s insurance plan.
Under HIPAA, providers must submit their Medicare Part A and B claims electronically using the ASC X12 standard transmission format, commonly known as HIPAA 5010. This is when the insurance company will process the claim, reviewing for covered services or procedures, and then accept or deny the claims. If there are errors, the claim will be denied, although a detailed explanation and steps to rectify any issues will be included. By having a clear itemization of medical services, you’ll reduce errors and streamline the process.
Verify Patient Insurance and Fiscal Responsibility
- Copayments are always collected at the point of service, but it’s up to the provider to determine whether the patient pays the copay before or immediately after their visit.
- The encounter form relays to the charge entry staff what services and procedures were performed and why they were performed.
- Timely submission and diligent follow-up are essential to ensure prompt payment.
- Verify that you have the case’s insurance information up to date and accurate during enrolment.
Articles similaires
- What Is Bookkeeping? Duties, Pay, and How to Become a Bookkeeper
- Transfer Pricing Definition, Example, Benefits, Risks
- Clinical management of alcohol withdrawal: A systematic review PMC
- Durham, NC Medical Marijuana Card Medical Marijuana Doctors
- What Is So Fascinating About Marijuana News?